A range of problems remain to be solved, however, not least the biocompatibility of blood vessels and the resilience of bioprinted organs. Researchers at the University of Edinburgh aim to tackle those problems – and their solution involves some humble components.
A £99 do-it-yourself 3D printer kit bought from Amazon forms the basis of a novel platform developed by the Edinburgh team, which has successfully built artificial blood vessels that closely mimic the properties of human veins.
“We deliberately made this very cheap,” said the project’s principal investigator, Dr Norbert Radacsi, to Professional Engineering. “One reason was because we didn't get any funding for this study. Second, also we wanted it generally to be accessible for low-income countries.”
Cardiovascular disease is the leading cause of death in the world. Many people die because of blocked arteries – especially the artery that surrounds the heart, called the coronary artery. As the coronary artery branches around the heart it gets smaller, so the researchers identified a need for small diameter vascular grafts for heart bypass surgery.
The team hopes the strong, flexible tubes could improve outcomes for patients by replacing the human and synthetic veins currently used in surgery to re-route blood flow. They believe the new vessels could help limit scarring, pain, and infection risk associated with the removal of human veins in bypass operations, 20,000 of which are carried out in England each year.
The products could also help alleviate the failure of small synthetic grafts, which can be hard to integrate into the body due to the immune response. The team hopes their new option, which uses modified gelatine from pigs, could be more compatible.
Printing platform
The Edinburgh team heavily modified the DIY 3D printer kit to build the platform. Instead of the conventional melting filament head, they added one capable of printing biological materials. They also replaced the bed with a rotating platform, which holds the mandrel around which the printer constructs the inner layer of the tubes.
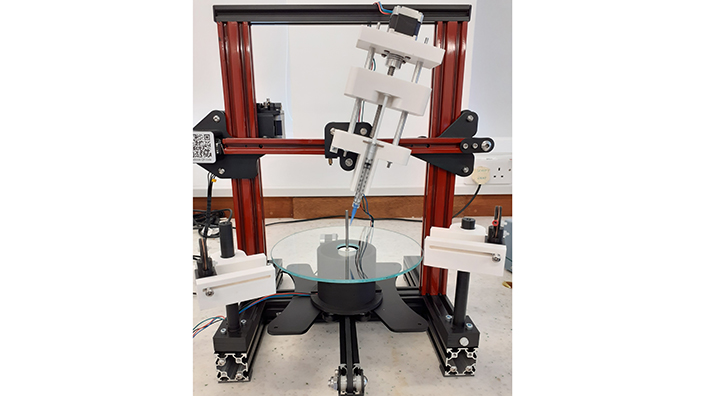
The 3D printer set-up
The system prints tubular grafts made from the modified gelatine hydrogel, which makes up the majority of the vessels. The printed graft is then reinforced with electrospinning, which uses high voltage to draw out very thin nanofibres, coating the artificial blood vessel in biodegradable polyester molecules.
The graft can be made with diameters of 1-40mm, which the team said should make them suitable for a range of applications. Tests showed the artificial products to be as strong as natural blood vessels.
The researchers also hope to include human cells in future. These would include human endothelial cells in the inner lining, then a layer of smooth muscle cells, replicating the structure of natural arteries.
Both the hydrogel and the polymers used in the current method will gradually degrade within the body in about two years, said Dr Radacsi, from the school of engineering. In future versions with human cells, those would be left behind.
When people think of polymers, they think of plastics – but Dr Radacsi said there should be no risk of microplastic contamination as they degrade. “This has been studied, and I can confirm that both of our polymers are fully degrading and they are not causing any toxicity or any problem,” he said.
“I worry about microplastics in general, because I know that there are plastics that never degrade. But since these polymers degrade within two years fully, I wouldn't worry about it.”
Removing bottlenecks
The variable thickness and branching of the printed vessels could also make them suitable for bioprinted organs such as kidneys in future, Dr Radacsi hopes, or the entire coronary artery branch system. The researcher said he is yet to see any useful 3D-printed organs despite over a decade of research, and mechanical properties are a “bottleneck”.
“For that we need to reinforce the hydrogels,” he said. “Because of the internal pressure… let's say you make a 3D-printed kidney without reinforcement, just hydrogel, then it will break into small pieces. And also from the pressure within the printed organ, because again you have pressure.”
He added: “If you reinforce it with something, a continuous nanofibre mesh for instance, then we have shown in our study that it can have the same mechanical properties as a young person's artery, vein, or a kidney or bladder in future.”
Dr Radacsi aims to explore artificial vessels with human cells, and bioprinted organs, in future research. He hopes to secure industry involvement and funding for the different topics.
The next stage of the current project will involve testing the 3D-printed blood vessels in animals in collaboration with the university’s Roslin Institute, followed by trials in humans. Animal testing in pigs could take place in five years, Dr Radacsi estimated, followed by human tests another five years after that.
The research, published in Advanced Materials Technologies, was carried out in collaboration with Heriot-Watt University. The lead author from the University of Edinburgh was Dr Faraz Fazal.
Want the best engineering stories delivered straight to your inbox? The Professional Engineering newsletter gives you vital updates on the most cutting-edge engineering and exciting new job opportunities. To sign up, click here.
Content published by Professional Engineering does not necessarily represent the views of the Institution of Mechanical Engineers.