Even if doctors are aware of a patient’s condition, it is not always possible to provide long-lasting treatment. Heart transplants offer a route to a longer, healthier life, but not everyone who needs one receives one. More than 5,000 heart transplants are performed each year, according to the International Society for Heart and Lung Transplantation – but an estimated 50,000 people need them.
Many of those patients will rely on artificial replacements while they wait. These can offer a vital stopgap, lengthening and improving the quality of patients’ lives. They have their own issues, however, including the risk of infection and blood clots.
Team Bath Heart wants to change that. The group of students from the University of Bath aims to create an improved ‘total artificial heart’, using wireless power and 3D printing to overcome common challenges associated with existing devices.
“Heart transplants aren't readily available, obviously, for patients. So we are creating a technology that would replace that, temporarily, as a bridge to transplant,” says leader Mansi Ahuja to Professional Engineering.
The team – from a range of disciplines, including mechanical and electrical engineering, biology and business studies – recently competed in the Heart Hackathon in Japan, coming out on top for the second year running.
Now, they are continuing development of their winning device. One day, they hope, it could even become a permanent replacement.
Preventing blood trauma
One of the main limitations with existing devices, according to mechanical lead Molly Holmes, is that they are not fully implantable. Even if a total artificial heart is installed in the chest, replacing the left and right ventricles, they rely on ‘drive lines’ into the body, connected to external power sources.
Often exiting the body through the skin of the abdomen, the lines are a “prime site for infection”, says Holmes. The team set out to counter that risk by making the device fully implantable, which involved developing a wireless power transfer system.
“By eliminating everything that goes through the skin, we want to really reduce the risk of infection,” says Dr Katharine Fraser, senior lecturer in mechanical engineering and lead academic advisor. “The Team Bath total artificial heart is powered electrically but wirelessly, eliminating any cuts or incisions through the skin after the surgery.”
The team is unable to say too much about the internal blood pumping mechanism for intellectual property reasons, but they say it differs from the impellers used in other devices over concerns about ‘blood trauma’ – damage to the red blood cells and other components from the forces within circulatory devices.
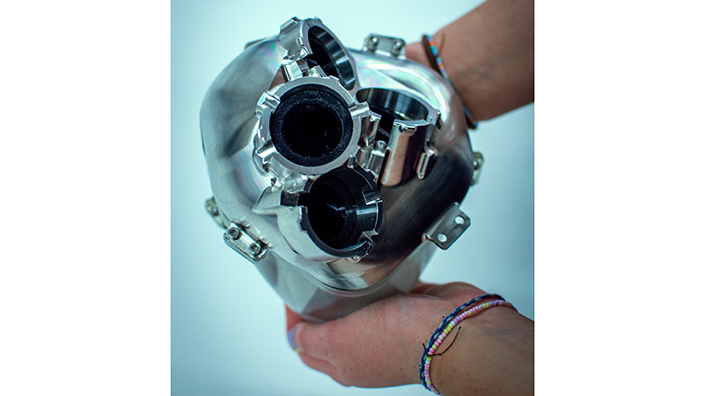
Team Bath Heart's prototype device
“We don't really know what negative effects this will then have on the blood,” Holmes says. “We’ve designed our device to be as haemocompatible as possible, and emulate the native heart as best we can.”
This involves using artificial ventricles, which Holmes describes as “sack shapes made out of polyurethane, and then we use sort of a plate compression mechanism to squeeze these, and then this ejects blood around the body.”
The students are also working on an active control system that uses sensors to monitor and adjust the heart rate accordingly. This would enable users to take part in more activities than they would otherwise be able to.
Virtual anatomy
Despite the aim of replicating the heart’s conditions as closely as possible, the device’s external appearance is clearly not biological, with a shiny metal casing.
Autodesk, one of the project’s sponsors, 3D-printed a version of the casing out of clear resin. They also machined the top plate – the upper part, with the tubes for connections – out of stainless steel. The team aims to eventually make it out of titanium, which is often used in medical devices for its biocompatibility.
The surgical procedure was a top consideration during development of the casing, so the team spoke to a heart surgeon and total artificial heart specialist for expert advice.
They also used software to investigate the virtual anatomy of some patients, and decided on a ‘target patient’ with particular weight and height. They then looked at the connection points they would need, to meet the aorta and the upper atrium.
“We were able to see where we'd make dissections and take measurements so we could fit our casing to this, so that's where the interesting tube shapes come from,” says Holmes.
“Then we designed components to actually attach the device to the body as well, and thought about the sealing, and trying to make the attachments as quick and easy as possible for surgeons.”
The team machined all of the internal components, getting a working prototype that pumps fluid. They also built a ‘mock circulatory loop’ (MCL) test rig to validate and prove the design, testing the pressure and flow produced by the device. That work is continuing, to garner more useful data.
To test whether their wireless power transfer system can safely power the device, the team is testing power outputs in a ‘phantom’, which replicates the skin, fat and muscle layers of the body. The control system is in early stages of development, Ahuja says.
Novel design
Having started with just six mechanical engineering students two years ago, the team now has more than 70 members. Their success in Japan on 12 November came against teams from the US, Australia, New Zealand, Romania, Egypt, Thailand and Sweden. Taking part alongside the International Society for Mechanical Circulatory Support (ISMCS) conference, the competition took place in Utsunomiya, north of Tokyo.
“I think what made us stand out was that we have a novel design that uses bags and doesn't have contact with the blood, and we were also quite far along ahead in our testing and our prototyping stages, and we were able to show that quite well,” says Ahuja.
They hope to patent their design but the first step is to make the design smaller, after already shrinking it down from the previous year’s entry.
“The main goal is to make it fit in a patient, because at the moment it's slightly too big,” says Ahuja. “There's obviously changes that we need to make, of the internal components and the external, and then hopefully get that manufactured again.”
Tests on the MCL would come after that, potentially followed by animal trials. If the device reaches clinical deployment, it could “make a huge impact”, according to Ahuja. “The one that we're producing has a lot of selling points, differences to the ones that are currently available, and they really take into account the user needs, and the user comfort and quality of life.”

Around the world, 64 million people have heart failure, says Dr Fraser. “Most of those, you would hope to treat with other methods – drugs, pacemakers. But heart failure is a degenerative disease, so the heart just keeps getting worse and worse.”
She adds: “For some people, it just gets to the point where they really, really need a new heart. Obviously, a total artificial heart is a drastic solution, and you're only going to do it in somebody where there's no other option. But at the moment, if someone can't get a heart transplant, then there really is no other option. And there is this group of patients who will die if they don't have something to replace their heart.
“So this is a potential technology which could really make a difference to those people.”
Even looking at upcoming devices, she says, “we think that Team Bath Heart will still be a better design due to the way we've really taken onboard the interaction with the body at the macro scale and producing the pulsatile flow, and also at the small scale, with the effects on the blood and the lack of infection.”
If it succeeds as a temporary device thanks to those advantages, they hope the device could eventually become ‘destination therapy’ – a permanent replacement for the heart.
The team received a travel grant from IMechE, as well as support from Ansys, Autodesk, Keysight, 3P Innovation and the Sasakawa Foundation.
Want the best engineering stories delivered straight to your inbox? The Professional Engineering newsletter gives you vital updates on the most cutting-edge engineering and exciting new job opportunities. To sign up, click here.
Content published by Professional Engineering does not necessarily represent the views of the Institution of Mechanical Engineers.